Diabetes is one of the most common diseases worldwide, and each passing year leaves behind a concerning global statistic. Shockingly, in India, the prevalence of diabetes among people under the age of 40 has increased by 50% in recent years.
This lifelong metabolic disorder impairs your body’s ability to process blood glucose (sugar) and causes you to have high levels of sugar in the blood. There are three main types of diabetes—- Type 1 (insulin-dependent), Type 2 (non-insulin-dependent), and gestational diabetes.
However, Type 2 diabetes is the most common form among all types. About 90 to 95 percent of people with diabetes are living with Type 2 diabetes. Keep reading for an in-depth look at what Type 2 diabetes is, its symptoms, and effective management strategies.
What Causes the Development of Type 2 Diabetes?
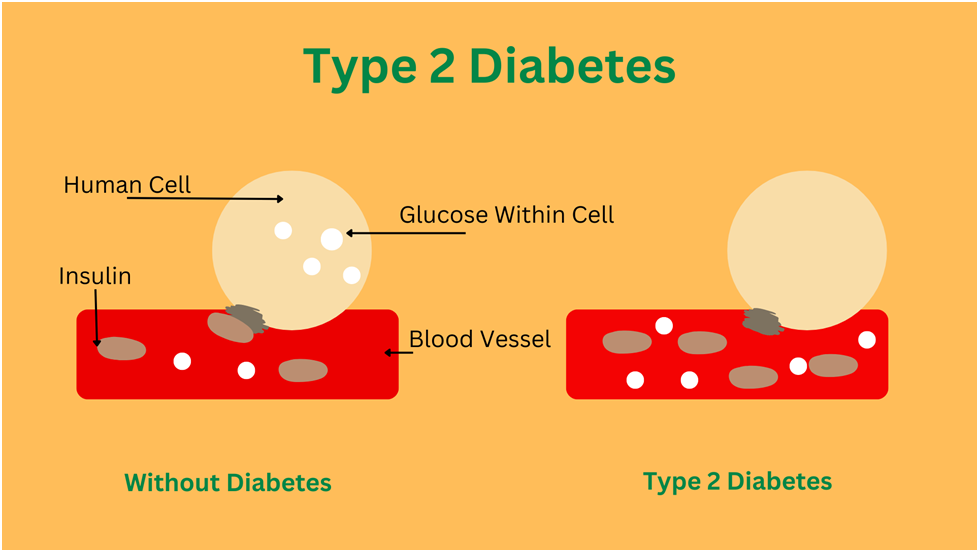
Primarily, insulin resistance is the cause of type 2 diabetes. This means your body is unable to use insulin properly. It is a hormone produced by your pancreas that controls or regulates the amount of sugar in your blood.
When you consume food and drinks, the carbohydrates that come from it are utilized by cells in your muscles, fat and liver for energy. Insulin is the key that helps in this process.
In type 2 diabetes even though your pancreas makes insulin, the cells do not respond to it like they should. They become resistant to insulin signals, so the sugar stays in your blood instead of moving into the cells to provide energy. This is why you always feel tired when dealing with diabetes because your cells aren’t getting the fuel they require.
Over time, when your body does not respond to insulin properly, your pancreas tries to make more insulin to keep up with the increasing blood glucose levels. Eventually, it can’t make enough to lower blood sugar effectively.
Insulin resistance can occur due to factors like:
- Genetics (family history)
- Being overweight
- Not being active enough
- Having an unhealthy diet with too much sugary or processed foods
- Using certain medications, like corticosteroids
- Hormonal disorders, including hypothyroidism and Cushing syndrome
- Chronic stress
- Lack of quality sleep
According to research, individuals over the age of 45 who have a family history of diabetes or are obese are more likely to develop Type 2 diabetes.
Though Type 2 diabetes mainly affects adults, children and teens can also develop it, often due to childhood obesity.
Early Signs of Type 2 Diabetes
Type 2 diabetes symptoms often develop gradually over several years and can easily be overlooked because they can be so mild that you might not even notice them. Initial symptoms might include:
- Lack of energy
- Unusual hunger
- Persistent thirst
- Frequent urination
- Unexpected weight loss
- Blurred vision
- Sores and cuts that heal slowly
- Gum disease
- Recurrent yeast or fungal infections
As Type 2 diabetes advances, symptoms can worsen over time and lead to serious health problems like diabetic eye disease (retinopathy), nerve damage causing tingling, numbness, or pain in the hands and feet (neuropathy), and kidney damage (nephropathy). People with diabetes are at twice the risk of heart disease and stroke, and nearly two-thirds also develop high blood pressure.
Also Read: 10 Early Signs of Diabetes That Shouldn’t Be Ignored
How is Type 2 Diabetes Diagnosed?
According to the American Diabetes Association, Type 2 diabetes can be diagnosed with any of these tests:
A1C Test: This blood test provides information about your average blood sugar levels over the past two to three months. An A1C of 6.5% or more indicates diabetes, 5.7% to 6.4% shows prediabetes and less than 5.7% is normal.
Fasting Plasma Glucose (FPG) Test: Checks your blood sugar levels following an eight-hour fast, usually in the morning. A result of 126 mg/dL or greater shows that you have diabetes.
Oral Glucose Tolerance Test (OGTT): Measures blood sugar two hours after drinking a sugary beverage. A value of 200 mg/dL or above suggests diabetes.
Random plasma glucose test: If you have symptoms of high blood sugar. this test can also be done at any time of the day without fasting. A result above 200 mg/dl may indicate diabetes.
Treatment for Type 2 Diabetes
Management of type 2 diabetes involves several strategies including lifestyle changes (healthy eating and regular exercise) blood sugar monitoring and diabetes medications.
Lifestyle Changes for Type 2 Diabetes
Working closely with your doctor, you can implement these five key lifestyle interventions to manage your diabetes.
1. Eat Healthy
What you eat, when you eat and how much you eat, are all crucial to keep your blood sugar levels within a healthy range. To reduce the risk of type 2 diabetes, the National Institute for Health and Care Excellence recommends eating more high-fibre foods and decreasing the intake of fat.
If you’re overweight, eat smaller portion sizes to cut down on calories. Focus on eating plenty of non-starchy vegetables, like green beans, broccoli, salad greens, cucumbers., and fruits. Consume more whole grains and lean protein. Limit the foods that are high in sugar and refined carbohydrates.
2. Exercise
If you have not been active yet, now is the time to start. You don’t need to join a gym or do intense workouts. Simple regular activities like brisk walking, biking, or playing your favourite sport for 30 minutes a day would be enough.
Being active for 5 days a week helps lower your blood sugar, reduces your risk of heart disease, helps you lose extra weight, and reduces stress.
3. Stay Stress-Free
Stress can cause your blood sugar levels to rise and make it difficult to manage your diabetes. When you’re anxious, you might forget to exercise, eat properly, or take your medications.
Find ways to reduce stress, such as deep breathing exercises, practising yoga, or engaging in relaxing hobbies.
4. Avoid Alcohol Consumption
Most alcoholic drinks are high in carbohydrates, which can make your blood sugar go too high. Alcohol also contains a lot of calories and causes weight gain, making it harder to manage diabetes.
5. Quit Smoking
Diabetes increases your risk of serious health issues such as heart disease, eye problems, stroke, kidney disease, nerve damage, and foot complications. Smoking further raises these risks.
Blood Sugar Monitoring
Your doctor will advise you on how frequently you should check your blood sugar to stay within the desired range. To check your blood sugar levels at home, you can use either a glucose meter and finger stick or a continuous glucose monitor (CGM).
Along with regular monitoring at home, it is also important to see your doctor at least twice a year. Diabetes increases your risk of heart disease especially if you have been facing it for years. Regular consultation with your doctor helps you keep track of your cholesterol levels, blood pressure and A1c (average blood sugar over three months) and know if the condition has taken over any other body organ.
Diabetes Medications
If you’re unable to achieve your target blood sugar level through diet and exercise alone, your doctor may prescribe medications that lower glucose levels or recommend starting insulin therapy.
Oral medications such as metformin, sulfonylureas, and DPP-4 inhibitors improve insulin sensitivity or increase insulin production helping to achieve the best blood glucose management.
Injectable medications like GLP-1 & dual GLP-1/GIP agonists are also prescribed in some cases to help regulate blood sugar levels and treat obesity.
Insulin therapy was used as a last resort in the past but today it may be prescribed earlier if blood sugar levels cannot be maintained with lifestyle modifications and other medications. Insulin directly helps in lowering blood sugar.
Ayurvedic medicines like Diabic Care Juice can also be used as a complementary treatment for diabetes management. It is a blend of 11 natural herbs. known to reduce blood sugar levels and prevent complications such as heart disease and high blood pressure.
Like any other chronic condition, Type 2 diabetes also demands constant self-care and making informed choices for effective management. Initially, it might seem like a daunting task, but with time, you’ll get a better grasp on managing the condition and understanding your body’s needs.
What are the common symptoms of Type 2 Diabetes?
Symptoms of type 2 diabetes are often mild and can develop gradually over the years. They may include:
- Frequent urination, particularly at night
- Increased thirst
- Persistent hunger
- Weight loss without trying
- Lack of energy
- Wounds and sores taking a longer time to heal
- Recurrent yeast or fungal infections
- Darkened areas of skin, usually on the neck and armpit
- Blurred vision
- Gum disease
As the condition advances it may affect other parts of the body and lead to serious health issues like tingling numbness or pain in the hands or feet (diabetic neuropathy), eye complications (diabetic retinopathy), kidney damage (nephropathy) and reduced sensations.
How is Type 2 Diabetes diagnosed?
To confirm the condition a series of blood tests are performed on different days that measure blood sugar levels. However, if your blood glucose levels are really high or you have several symptoms, a single test may be enough.
Blood tests for type 2 diabetes are:
- Fasting plasma glucose test: This lab test checks your blood sugar level on an empty stomach, usually in the morning after an eight-hour fast. A result of 126 mg/dL or higher on two separate tests indicates you have diabetes.
- A1C test: This is a common blood test that is used to measure your average blood sugar levels over the past 2-3 months. A result of 6.5% or higher on two separate tests means you have diabetes.
Oral glucose tolerance test (OGTT): This test is less common and is mostly used to diagnose diabetes during pregnancy. Your blood sugar levels are checked before and after 2 hours of drinking a sugary liquid to see how your body handles the sugar.
What causes Type 2 Diabetes?
Insulin resistance, a condition in which the cells in your muscles, fat and liver don’t respond to the hormone insulin properly is the main cause of type 2 diabetes.
This can occur due to several reasons. Lack of physical activity, being overweight or obese coupled with regular consumption of highly processed, high-carbohydrate foods, all can contribute to insulin resistance and faster progression from prediabetes to type 2 diabetes. Genetics or having a family history of diabetes, long-term medications like steroids, chronic stress and insufficient sleep can also cause insulin resistance in your body.
Is Type 2 Diabetes reversible?
With a little discipline and the correct support system, yes!
Though there is no complete cure for type 2 diabetes, it can be reversed in some people. With lifestyle adjustments like regular physical activity, improved diet, and sufficient sleep you can maintain your blood sugar levels in a healthy range. Remember, this does not offset the effects of Type 2 diabetes as it is an ongoing disease. So, even if you’re in remission, where your blood sugar levels are under control and you’re not taking any medications, there’s still the chance that symptoms can return. But, with the use of Ayurvedic products like Krishna’s Diabic Care Juice, it’s possible to go years without health issues associated with diabetes. You may also be able to reach and hold a point where medications are no longer needed.
Who is at risk for developing Type 2 Diabetes?
People who are more likely to develop type 2 diabetes than others include:
- Individuals who are overweight or struggle with obesity
- Someone having a parent, brother, or sister with type 2 diabetes
- People aged 45 or above
- Having a high waist measurement (men>40 inches/ 101.6 centimetres and women >35 inches/ 88.9 centimetres).
- A person who lacks fitness activities
- Women having a history of gestational/pregnancy diabetes
- People with high blood pressure
- Women who have PCOS (Polycystic ovary syndrome)
Can Type 2 Diabetes be prevented?
Yes, with early action and certain lifestyle changes, you can prevent or delay type 2 diabetes. Here are some strategies that can help to lower your risk.
- Make healthy eating choices and be mindful of your portion size
- Stay more physically active (exercise at least 30 minutes a day for 5 days a week).
- Maintain a healthy body weight or lose some weight if required
- Take care of your mental health and try to remain stress-free
Quit smoking and alcohol consumption
What are the treatment options for Type 2 Diabetes?
Managing type 2 diabetes includes a combination of lifestyle changes (eating well and exercising for weight loss), self-care strategies, and medications. Commonly prescribed medicine is Metformin which helps control blood sugar levels, as well as other drugs that boost insulin production or enhance insulin sensitivity.
How does Type 2 Diabetes affect daily life?
When you’re already juggling your job, family, and personal wellness, adding another challenge like diabetes can be daunting. Besides causing physical health issues, the condition can take a toll on your day-to-day life in various ways. It can lead to anxiety, depression, and frustration, making it challenging to stay focused or productive. The constantly high blood sugar levels can make you feel tired all day and cause mood swings making it difficult to manage routine tasks.